5 Key Indicators of Hemolysis in Lab Tests
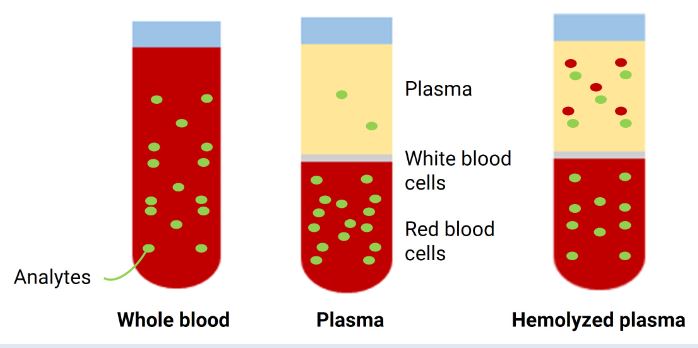
Hemolysis refers to the rupture of red blood cells (RBCs) and the release of hemoglobin into the bloodstream. This phenomenon can occur naturally or as a result of laboratory errors. In clinical diagnostics, identifying hemolysis in lab tests is critical, as it can significantly affect the accuracy of various test results. Detecting hemolysis involves recognizing certain key indicators that can provide valuable insights into the cause and extent of RBC breakdown. Below are five key indicators of hemolysis commonly observed in lab tests.
Five Key Indicators of Hemolysis Labs
Here are details about five key indicators of Hemolysis labs:
Visual Appearance of the Sample
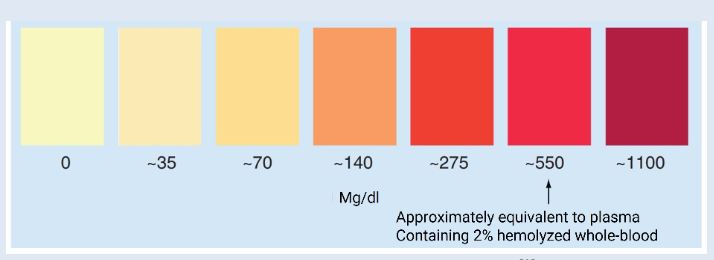
One of the most straightforward ways to detect hemolysis is by observing the visual appearance of the blood sample. When hemolysis occurs, the plasma or serum becomes pink or red, due to the presence of free hemoglobin released from the lysed red blood cells. This color change can vary depending on the extent of hemolysis. If the sample appears mildly pink, it suggests partial hemolysis, while a dark red or even brown discoloration could indicate more severe hemolysis. The visual assessment of the sample is often the first step in determining whether hemolysis has occurred, and it is crucial to identify this before proceeding with further analysis.
Increased Free Hemoglobin Levels
Hemoglobin is typically contained within red blood cells, but when these cells rupture during hemolysis, free hemoglobin is released into the blood plasma. This can be measured directly by laboratory tests that quantify the amount of free hemoglobin. Elevated levels of free hemoglobin in the plasma or serum are a strong indicator that hemolysis has occurred. High concentrations of free hemoglobin can interfere with a wide range of lab tests, including liver function tests, renal function tests, and potassium measurements, often leading to inaccurate results. Thus, detecting increased free hemoglobin can be crucial for flagging the possibility of hemolysis in lab results.
Altered Potassium Levels
Potassium is an important electrolyte present inside red blood cells. When hemolysis occurs, the potassium stored in RBCs is released into the bloodstream, which can lead to abnormally high potassium (hyperkalemia) levels. Elevated potassium levels are one of the most common laboratory findings associated with hemolysis. This alteration can be detected through standard blood tests that measure electrolyte concentrations. Hyperkalemia is significant because it can cause serious health problems, such as cardiac arrhythmias, if not properly managed. Therefore, the presence of elevated potassium levels should raise suspicion for hemolysis, especially if other indicators are also present.
Changes in the Serum or Plasma Chemistry
Hemolysis can also lead to alterations in various biochemical markers in serum or plasma. For instance, elevated levels of lactate dehydrogenase (LDH) and bilirubin can be indicative of hemolysis. LDH is an enzyme found inside red blood cells, and its release into the plasma occurs when the cells rupture. Therefore, increased LDH levels are often observed in hemolyzed samples. Similarly, the breakdown of hemoglobin during hemolysis results in the production of bilirubin, which can elevate the bilirubin levels in the plasma. Elevated LDH and bilirubin levels are critical indicators that help to confirm the occurrence of hemolysis and differentiate it from other potential causes of abnormal lab results.
Elevated Indirect Bilirubin
Indirect bilirubin, also known as unconjugated bilirubin, is a product of hemoglobin degradation. When red blood cells break down, the heme portion of hemoglobin is metabolized to produce indirect bilirubin, which is then processed by the liver. However, in the case of hemolysis, the large volume of hemoglobin released can overwhelm the liver’s capacity to process the bilirubin, leading to an increase in its levels in the blood. Elevated indirect bilirubin is often seen in patients with hemolysis and can be detected through routine liver function tests.
Conclusion
Hemolysis can occur in a variety of contexts, including physiological conditions, medical treatments, and laboratory procedures. Recognizing the key indicators of hemolysis labs tests ensure accurate diagnosis and effective clinical decision-making. Awareness of these indicators can help laboratory professionals and healthcare providers distinguish between true hemolysis and laboratory artifacts, ensuring more reliable test results and better patient care.